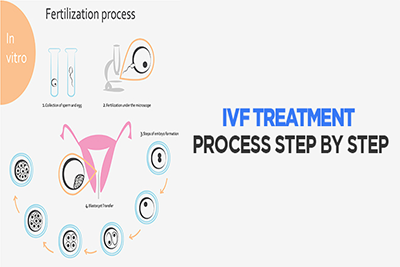
Understanding The IVF Treatment Step By Step
Understanding The IVF Treatment Step By Step
Starting IVF treatment can be an exciting but nerve wracking experience. Usually, IVF treatment is pursued once other treatments have failed, following months of trying to get pregnant unsuccessfully. IVF treatment is the very first treatment tried when an egg donor is being used, there are severe cases of male infertility or a woman’s fallopian tubes are blocked. Still, this often comes after years of trying to get pregnant, followed by a slew of fertility testing.
IVF treatment is often successful, though, it may take more than one try. Studies show that the potential for success with IVF treatment is the same for up to four cycles. Generally, the live birth rate for each IVF cycle is 30 to 35% for women under age 35, 25% for women between the ages of 35 and 37, 15 to 20% for women between the ages of 38 and 40 and 6 to 10% for women after age 40. (When an egg donor is used, however, success rates remain high even at age 40, with a 45% success rate.)
If you’re feeling overwhelmed, don’t feel bad. IVF treatment is quite stressful. Just looking over the schedule of ultrasounds, blood work, injections and so on can have you feeling fragile. (And that’s before the drugs have a chance to mess with your moods!)
You may be wondering how everything will come together. While every clinic’s protocol will be slightly different and treatments are adjusted for a couple’s individual needs, here is a step-by-step breakdown of what generally takes place during an IVF treatment cycle.
IVF Treatment Step One: The Cycle Before Treatment
The cycle before your IVF treatment is scheduled, you may be put on birth control pills. This may seem backward — aren’t you trying to get pregnant? Actually, though, using birth control pills before a treatment cycle has been shown to decrease your risk of ovarian hyperstimulation syndrome and ovarian cysts and may even improve the odds of success.
Another possible option your doctor may ask you to look out for is going by your ovulation (either by basal body temperature charting or with an ovulation predictor kit). Let your doctor know as soon as you detect ovulation. Sometime after ovulation, the fertility clinic may then have you start taking a GnRH antagonist or a GnRH agonist, such as Lupron. This is so they can have complete control over ovulation once your treatment cycle begins.
Another possibility, if you rarely get cycles on your own, is taking progesterone to bring on your period. In this case, your doctor will probably ask that you start taking the GnRH agonist or antagonist about six days or more after your first pill. Again, though, this may vary. Always follow your doctor’s instructions.
IVF Treatment Step Two: When You Get Your Period
The first official day of your treatment cycle is the day you get your period. (Even though it may feel like you’ve already begun with the medications you’ve started before in step one.) On the second day of your period, your doctor will likely order blood work and an ultrasound. (Yes, an ultrasound during your period isn’t exactly pleasant, but what can you do?) This is referred to as your baseline blood work and your baseline ultrasound.
In your blood work, your doctor will be looking at your estrogen levels, specifically your E2 or estradiol. This is to make sure your ovaries are “sleeping,” the intended effect of the Lupron shots or GnRH antagonist.
The ultrasound is to check the size of your ovaries, and look for ovarian cysts. If there are cysts, your doctor will decide how to deal with them. Sometimes your doctor will just delay treatment for a week, as most cysts will resolve on their own with time. In other cases, your doctor may aspirate, or suck, the cyst with a needle. Usually, these tests will be fine. If everything looks OK, treatment moves on to the next step.
IVF Treatment Step Three: Ovarian Stimulation And Monitoring
If your blood work and ultrasounds look normal, the next step is ovarian stimulation with fertility drugs. Depending on your treatment protocol, this may mean anywhere from one to four shots every day, for about a week to 10 days. (Ouch.)
During ovarian stimulation, your doctor will monitor the growth and development of the follicles. At first, this may include blood work every few days, to monitor your estradiol levels, and ultrasounds, to monitor the oocyte growth. Monitoring the cycle is important, as it helps your doctor decide whether or not the medications need to be increased or decreased in dosage. Once your largest follicle is 16 to 18mm in size, your clinic will probably want to see you daily.
IVF Treatment Step Four: Final Oocyte Maturity
The next step in your IVF treatment is triggering the oocytes to go through the last stage of maturation, before they can be retrieved. This last growth is triggered with human chorionic gonadotropin (hCG). Brand names for this include Ovidrel, Novarel and Pregnyl.
Timing this shot is vital. If it’s given too early, the eggs will not have matured enough. If given too late, the eggs may be “too old” and won’t fertilize properly. The daily ultrasounds at the end of the last step are meant to time this trigger shot just right. Usually, the hCG injection is given when four or more follicles have grown to be 18 to 20mm in size and your estradiol levels are greater than 2,000pg/ML.
This shot is typically a one-time injection (yeah!). The timing of the shot will be based both on your ultrasounds and blood work and when your clinic schedules your retrieval. If not enough follicles grow or if you’re at risk for severe ovarian hyperstimulation syndrome, your treatment cycle may be canceled and the hCG shot will not be given. If treatment is canceled because your ovaries didn’t respond well to the medications, your doctor may recommend different medications to be tried on the next cycle.
While not common, a cycle may also be canceled if ovulation occurs before retrieval can take place. Once the eggs ovulate on their own, they can’t be retrieved.
Cancellation happens in 10 to 20% of IVF treatment cycles. The chance of cancellation rises with age, with those older than age 35 more likely to experience treatment cancellation.
IVF Treatment Step Five: Egg Retrieval
About 34 to 36 hours after you receive the hCG shot, the egg retrieval will take place. It’s normal to be nervous about the procedure, but most women go through it without much trouble or pain.
Before the retrieval, an anesthesiologist will give you some medication intravenously to help you feel relaxed and pain free. Usually, a light sedative is used, which will make you “sleep” through the procedure. This isn’t the same as general anesthesia, which is used during surgery. Side effects and complications are less common.
Once the medications take their effect, your doctor will use a transvaginal ultrasound to guide a needle through the back wall of your vagina, up to your ovaries. She will then use the needle to aspirate the follicle, or gently suck the fluid and oocyte from the follicle in to the needle. There is one oocyte per follicle. These oocytes will be transferred to the embryology lab for fertilization.
The number of oocytes retrieved varies but can usually be estimated before retrieval via ultrasound. The average number of oocytes is 8 to 15, with more than 95% of patients having at least one oocyte retrieved.
After the retrieval procedure, you’ll be kept for a few hours to make sure all is well. Light spotting is common, as well as lower abdominal cramping, but most feel better in a day or so after the procedure. You’ll also be told to watch for signs of ovarian hyperstimulation syndrome, a side effect from fertility drug use during IVF treatment in 10% of patients.
IVF Treatment Step Six: Egg Fertilization
While you’re at home recovering from the retrieval, the follicles that were aspirated will be searched for oocytes, or eggs. Not every follicle will contain an oocyte.
Once the oocytes are found, they’ll be evaluated by the embryologist. If the eggs are overly mature, fertilization may not be successful. If they are not mature enough, the embryology lab may be able to stimulate them to maturity in the lab.
Fertilization of the oocytes must happen with 12 to 24 hours. Your partner will likely provide a semen sample the same morning you have the retrieval. The stress of the day can make it difficult for some, and so just in case, your partner may provide a semen sample for backup earlier in the cycle, which can be frozen until the day of the retrieval.
Once the semen sample is ready, it’ll be put through a special washing process, which separates the sperm from the other stuff that is found in semen.
The embryologist will choose the “best looking sperm,” placing about 10,000 sperm in each culture dish with an oocyte. The culture dishes are kept in a special incubator, and after 12 to 24 hours, they are inspected for signs of fertilization. With the exception of severe male infertility, 70% of the oocytes will become fertilized.
In the case of severe male infertility, ICSI (pronounced ick-see) may be used to fertilize the eggs, instead of simply placing them in a culture dish. With ICSI, the embryologist will choose a healthy-looking sperm and inseminate the oocyte with the sperm using a special thin needle.
IVF Treatment Step Seven: Embryo Transfer
About three to five days after the retrieval, the fertilized eggs will be transferred. The procedure for embryo transfer is just like IUI treatment. You won’t need anesthesia.
During the embryo transfer, a thin tube, or catheter, will be passed through your cervix. You may experience very light cramping but nothing more than that. Through the catheter, they will transfer the embryos, along with a small amount of fluid.
The number of embryos transferred will depend on the quality of the embryos and previous discussion with your doctor. Depending on your age, anywhere from two to five embryos may be transferred. Recent studies have shown success with just one embryo transferred. Speak to your doctor to find out if this may apply to you.
After the transfer, you’ll stay lying down for a couple hours (bring a book) and then head home.
If there are “extra” high-quality embryos left over, you may be able to freeze them. This is called embryo cryopreservation. They can be used later if this cycle isn’t successful, or they can be donated.
IVF Treatment Step Eight: Progesterone Support And The Two Week Wait
On or after the day of your retrieval, and before the embryo transfer, you’ll start giving yourself progesterone supplements. Usually, the progesterone during IVF treatment is given as an intramuscular self-injection as progesterone in oil. (More shots!) Sometimes, though, progesterone supplementation can be taken as a pill, vaginal gel or vaginal suppository.
Besides the progesterone, there really isn’t much going on for the next two weeks. In some ways, the two weeks after the transfer may be more difficult emotionally than the two weeks of treatment. During the previous steps, you will have visited your doctor perhaps every other day. Now, after transfer, there will be a sudden lull in activity.
You may have lots of questions about the two week wait. Can you have sex? What if you have cramps? Of course, your doctor is the number one source for any of your concerns.
All you can do is wait the two weeks and see if pregnancy takes place. It can help to keep busy with your life during this wait time and avoid sitting and thinking about whether or not treatment will be successful.
IVF Treatment Step Nine: Pregnancy Test And Follow-Up
About nine to twelve days after the embryo transfer, a pregnancy test is ordered. This is usually a serum pregnancy test (more blood work) and also will include progesterone levels testing. The test may be repeated every few days.
If the test is positive (yeah!), you may need to keep taking the progesterone supplementation for another several weeks. Your doctor will also follow up with occasional blood work and ultrasounds to monitor the pregnancy and watch for miscarriages or ectopic pregnancies.
During IVF treatment, miscarriage occurs up to 15% of the time in women under age 35, 25% of women age 40 and up and 35% of the time after age 42.
Your doctor will also monitor whether or not the treatment led to a multiple pregnancy. If it’s a high-order pregnancy (4 or more), your doctor may discuss the option of reducing the number of fetuses in a procedure called a “multifetal pregnancy reduction”. This is sometimes done to increase the chances of having a healthy and successful pregnancy.
What To Expect During Early IVF Pregnancy When IVF Treatment Fails
If the pregnancy test is still negative 12 to 14 days post-transfer, however, your doctor will ask you to stop taking the progesterone, and you’ll wait for your period to start. The next step will be decided among you, your partner and your doctor.
Having a treatment cycle fail is never easy. It’s heartbreaking. It’s important, however, to keep in mind that having one cycle fail doesn’t mean you won’t be successful if you try again.